The Emergency Department Error Detection System (EEDS) is a system intended to identify and avert potential medical errors in the Emergency Department. In addition, it has the ability to detect combinations of clinical and demographic data (e.g., clinical trial potential subject identification).
A recent report of the Institute of Medicine identified preventable medical errors as a significant cause of death in the United States. Many such events occur in the busy setting of the emergency department, and can often be attributed to limits in the clinical processes in which data associated with a patient is not available at the point of clinical contact. In addition, standards for identification of clinical abnormalities are not applied in a consistent manner.
An early prototype of the system was used in a retrospective analysis of medical charts, indicating a significant number of unresolved clinical abnormalities. This study led to the current project .
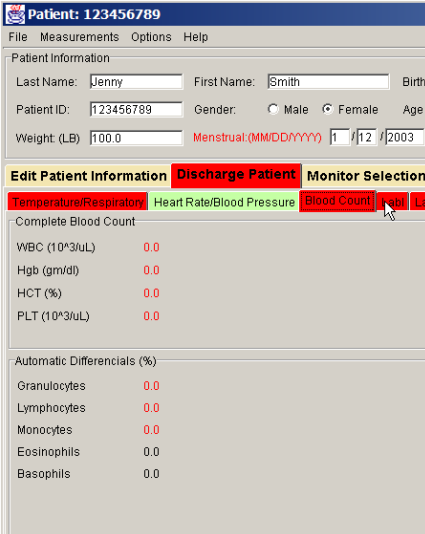
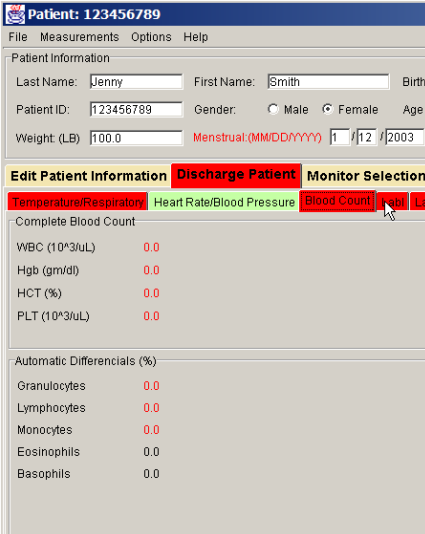
EEDS will enable many of these errors to be identified while it is still possible to avoid or correct them. The approach is to automatically collect clinical data and apply these data against a consistent set of clinical rules at the time of discharge. Any data that is outside normal ranges for the patient are identified on the user interface . The clinician can either act on the abnormality or ignore it, recording the reasons for either.
EEDS is composed of the following major components:
| Current Students |
|---|
| 2009-20010 |
|
The system is currently deployed in the Stony Brook Hospital Department of Emergency Medicine, and is currently being used to identify potential subjects for clinical trials. DUring the current academic year, the system will be modified to allow multiple libraries of rules, provide user selection of desired categories of alerts and allow rules that use streams of monitor data.
The system is being developed in collaboration with the Stony Brook Health Science Center (MSRC) and Dr. Adam Singer and has been supported with grants from the Emergency Medicine Foundation and the U.S. Department of Health and Human Services.